Asthma affects millions worldwide. While many patients respond well to inhalers and medications, some continue to experience severe symptoms despite optimal therapy. For these individuals, advanced interventions may be necessary. One such option is bronchial thermoplasty, a relatively new procedure designed to reduce airway constriction by targeting the muscles in the airway walls.
In this blog, we delve into bronchial thermoplasty how it works, the procedure itself, its benefits and risks, recovery expectations, and who may be an ideal candidate. Dr Kunal Waghray, a renowned pulmonologist in Hyderabad, provides expert guidance for patients considering advanced asthma care.
What is Bronchial Thermoplasty?
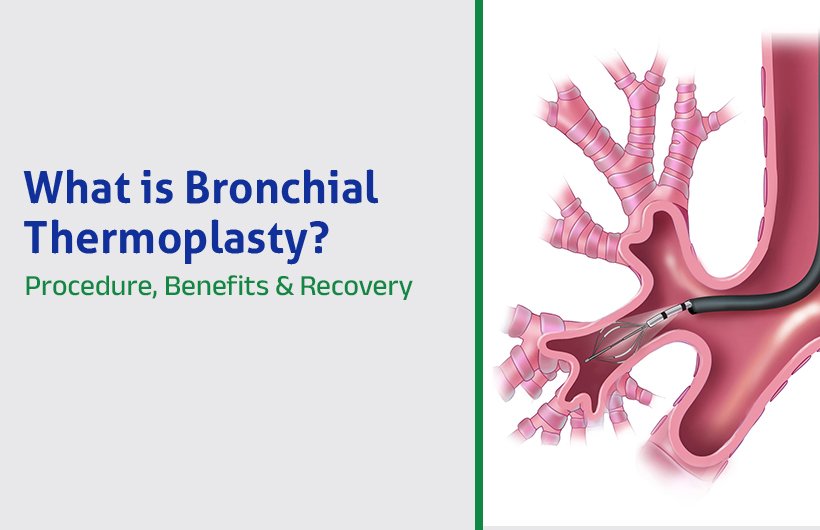
Bronchial thermoplasty (BT) is a bronchoscopic procedure designed to reduce the smooth muscle mass in the walls of the airways. Over time, in severe asthma, these airway muscles can thicken, making them more prone to constriction (narrowing). By applying gentle and controlled heat (via radiofrequency energy) to specific segments of the airway, bronchial thermoplasty aims to reduce this muscle bulk, making the airways less reactive.
It is essential to emphasise that bronchial thermoplasty is not a cure; patients will likely still require medication afterwards. Still, it may help reduce the intensity and frequency of asthma exacerbations in carefully selected cases.
How Does Bronchial Thermoplasty Work?
The principle behind BT is to reduce the contractile potential of airway smooth muscle, so that during an asthma trigger, the airways are less prone to constriction. Here’s how it works:
- A bronchoscope, a thin, flexible tube with a camera and working channel, is gently inserted through the mouth (or sometimes nose) and guided into the airways under light anaesthesia or sedation.
- Through the bronchoscope, a special catheter equipped with small electrodes is advanced. These electrodes expand to touch the airway walls.
- Radiofrequency energy is delivered in short, controlled bursts (e.g. about 10 seconds each) to heat the airway wall to a target temperature (around 65 °C). It is sufficient to affect the smooth muscle but not damage deeper structures.
- The heat reduces the amount of airway smooth muscle over time, making the airways less responsive to triggers that normally cause narrowing.
- The catheter and bronchoscope are withdrawn, and the treated airway segments are monitored.
Because it is not safe to treat all airways in a single session, the full bronchial thermoplasty treatment involves three separate procedures, spaced several weeks apart, each focusing on different lung regions (e.g., right lower lobe, left lower lobe, and both upper lobes together). The right middle lobe is typically avoided to reduce the risk of collapse.
Procedure of Bronchial Thermoplasty
Let’s walk through the steps of the procedure itself and what patients can expect before, during, and after.
Before the procedure
- You’ll be asked to fast (no food or drink) for several hours before the procedure.
- Often, a short course of oral steroids (e.g. prednisone) is given a few days before the procedure to reduce inflammation risk.
- You’ll be evaluated for fitness, and arrangements are made for a companion to take you home afterwards.
During the procedure
- Intravenous sedation or anaesthesia is used, so you are comfortable and minimally aware.
- The bronchoscope is navigated into the target airways.
- The radiofrequency catheter is deployed in each section, and controlled heating is applied to the airway wall.
- The procedure typically lasts about 45 minutes to an hour.
After the procedure
- You will be monitored for a few hours while waking up.
- Some patients may be discharged the same day, while others may need an overnight hospital stay if symptoms worsen.
- You’ll continue to have follow-up visits and lung function checks, especially after the final session.
Benefits of Bronchial Thermoplasty (Bronchial Thermoplasty Benefits)
Bronchial thermoplasty offers several potential advantages, especially for patients with severe asthma that is not well controlled:
- Fewer asthma exacerbations: Patients may experience fewer episodes requiring high-dose steroids or emergency intervention.
- Reduced emergency room visits and hospitalisations: Clinical studies have shown declines in the number of ER visits and admissions related to asthma.
- Improved quality of life: Many patients report fewer symptoms, less reliance on rescue medications, and fewer lost days from work or school.
- Durability of benefit: Studies following patients for up to 5 years show sustained benefit, stable lung function, and no worsening of safety signals over time.
- Reduction in muscle reactivity: The reduction in airway smooth muscle mass reduces the tendency of airways to constrict.
That said, bronchial thermoplasty is complementary to, not a replacement for, standard asthma medications. Most patients will continue inhaling or using other therapies even after undergoing BT.
Risks and Side Effects
As with any procedure, bronchial thermoplasty carries some risk. It is generally well tolerated, but patients should be aware of possible complications.
Common/short-term side effects
- Worsening asthma symptoms in the first few days: cough, wheezing, shortness of breath, chest discomfort.
- Fever, throat irritation, airway irritation.
- In rare cases, hospitalisation may be required for symptom management.
Serious risks (less common but important)
- Infection of the airways or lungs
- Collapse of part of a lung (atelectasis)
- Bronchiectasis or structural changes in rare cases
- In theory, bleeding or damage from bronchoscopy (though the risk is low).
Long-term data (up to 5 years) have not shown worsening in lung function or increased rates of hospital admissions beyond that expected, which supports the relative safety of the procedure in experienced hands.
Recovery After Bronchial Thermoplasty
What to expect in the first days
Patients may experience cough, wheezing, or mild shortness of breath in the first few days. These symptoms typically resolve within a week with appropriate care.
You should remain under observation for several hours of post-procedure, and some mild precautions are usually advised: rest, avoid strenuous activity, and adhere to your asthma medications.
Timeline for improvement
Some patients notice improvements in symptom control after their first session; for others, the full benefit may emerge only after all three sessions are complete.
Each procedure is spaced several weeks apart, and follow-up with lung function tests and clinical assessments helps monitor progress.
When to contact your doctor
You should seek immediate care if you experience:
- Persistent or worsening shortness of breath
- Chest pain
- Fever
- Coughing up blood
- Symptoms of asthma flare that do not improve with medication
With careful follow-up, most patients recover uneventfully and gain long-term benefits.
Who is an Ideal Candidate?
Bronchial thermoplasty is not suitable for everyone. Ideal candidates typically match the following profile:
- Adults (usually age 18 and above) with severe persistent asthma not adequately controlled by high-dose inhaled corticosteroids, long-acting bronchodilators, or even biologic therapies.
- Frequent exacerbations or hospital/ER visits despite maximal therapy.
- Good lung function (often with FEV₁ above a threshold) and ability to undergo bronchoscopy safely.
Contraindications or caution may include:
- Individuals with significant comorbidities make bronchoscopy unsafe
- Those with implanted electronic devices like pacemakers or defibrillators
- Known allergies or sensitivity to medications used during bronchoscopy or sedation
- Previous BT treatment (you generally do not repeat the procedure)
Conclusion
Bronchial thermoplasty offers a promising solution for patients with severe asthma that does not respond to standard treatments. By applying controlled heat to the airway walls, the procedure reduces smooth muscle mass, lessening the tendency of the airways to constrict. Typically performed over three sessions, each lasting 45 to 60 minutes, bronchial thermoplasty has been shown to decrease asthma exacerbations, reduce hospitalisations, and improve overall quality of life for many patients.
If controlling your asthma remains a challenge despite high-dose inhalers or biologics, it may be time to consider advanced treatment options. Consult a asthma specialist in Hyderabad, like Dr Kunal Waghray, who can assess your suitability, guide you through the process, and perform the procedure with precision and care.